
Sudden death of young athletes
Although very rare (approximately 3 cases per 100,000 athletes per year), the sudden death of young athletes is a serious health problem.
Sudden death on the sports field is a tragic event that deeply shakes the family, other athletes, institutions (schools, universities or professional associations), sports health workers and the community.
When it happens, it is heavily featured in the media because young athletes are considered the healthiest part of the population, and are often seen as heroes. Instinctively, everyone's first thought is whether there is an intervention that could prevent the sudden death of athletes.
The most common causes of sudden cardiac death (SCD) on the sports field are heart muscle diseases (cardiomyopathy), coronary artery diseases, some syndromes and cardiac arrhythmias.
Many of these diseases can be asymptomatic and sudden cardiac death is often the first and only manifestation of the disease.
The risk of sudden death increases with age and is more common in male athletes.
Young athletes are by definition individuals aged 12 to 35, who regularly train and participate in official sports competitions.
Athletes at risk of SCD are identified through preventive cardiovascular examinations, in an authorized health institution, by a sports doctor.
First, in a large population of athletes, seemingly healthy athletes who may have a life-threatening cardiovascular disease (CVD) are separated from those who may not. This is achieved by testing based primarily on ECG.
It is crucial that the selection of potentially healthy and potentially unhealthy athletes is carried out by competent and experienced sports doctors (sports medicine specialist or sports cardiologist), primarily for two reasons:
- The first is to avoid serious health consequences - unjustified exclusion from competition or misinterpreting a potentially deadly heart disease as a normal variant of a sports heart.
- The second is to avoid costly medical examinations due to excessive referral to further, otherwise, more expensive diagnostic tests. The percentage of false-positive findings (athletes with a normal heart but a positive result) should not exceed 9% for the prevention program to be sustainable.
Further examination (usually ultrasound of the heart) of those with a positive or suspicious test should rule out or diagnose a CVD and prevent SCD on the sports field through appropriate treatment.
The medical examination algorithm is given in Table 1.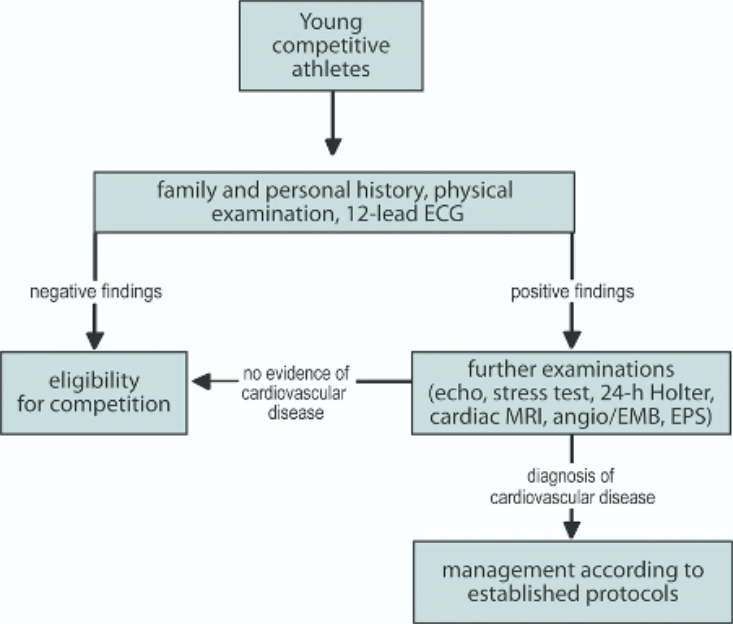
Table 1.
The manner in which the health of athletes is determined in order for them to safely participate in sports competitions depends on the specifics of the health system, socio-economic circumstances and cultural characteristics of each country.
Thus, for example, in USA, a strategy is in place that includes medical history (personal and family) and physical examination, without a 12-channel ECG or other tests. Most European Cardiac Societies and Sports Medical Federations have adopted ECG-based prevention, which is also recommended by the International Olympic Committee.
Twenty-five years of experience in applying one such screening in Italy has unequivocally shown that the introduction of ECG has led to a significant reduction (up to 89%) of the SCD of athletes in this country. Despite this, the professional public around the world is still debating the optimal prevention of sudden cardiac death in athletes.
What is the situation in Montenegro?
First of all, the care for the health of athletes is regulated by the "Rulebook on the conditions for performing health examinations of athletes", from 2015. This rulebook was written on the basis of the Law on Sports from 2013, which is no longer in force.
According to the Rulebook, health examinations should be performed in an "authorized health institution", and according to the current law from 2018, in a specially established institution that has not yet commenced its operation.
The question arises where amateur athletes, child athletes and professional athletes should be examined. It is also questionable whether the health institutions where medical examinations of athletes are currently performed can provide the necessary quality and scope of health services as prescribed by the Rulebook/Law.
