When children complain of chest pain, the least likely scenario is that the pain comes from the heart. A more common reason is pain from the muscles and bones/ribs of the rib cage, stomach or respiratory tract organs (bronchi, lungs ...).
The child usually comes to the clinic when they complain about "a throbbing pain" or "as if someone stabbed them with a knife", with this unpleasant feeling lasting for a short amount of time and the child can locate it with their finger.
The probability of such pain coming from the heart is low, especially if the pain occurs in a certain body position, when moving or pressing with a finger.
Pain originating from the heart is usually in the wider chest area and is described as burning, tearing, or pressure in the chest. They most often occur during physical activity when they can be accompanied by rapid fatigue, a feeling of irregular heartbeat, dizziness, and even loss of consciousness. If someone in the family had a congenital heart defect or died suddenly, then there is a great chance that a heart disease could be the culprit.
When talking to the child and their parents, the doctor should always ask under what circumstances (previously healthy or sick child) the pain occurred, how often it occurs and whether something provokes or alleviates it.
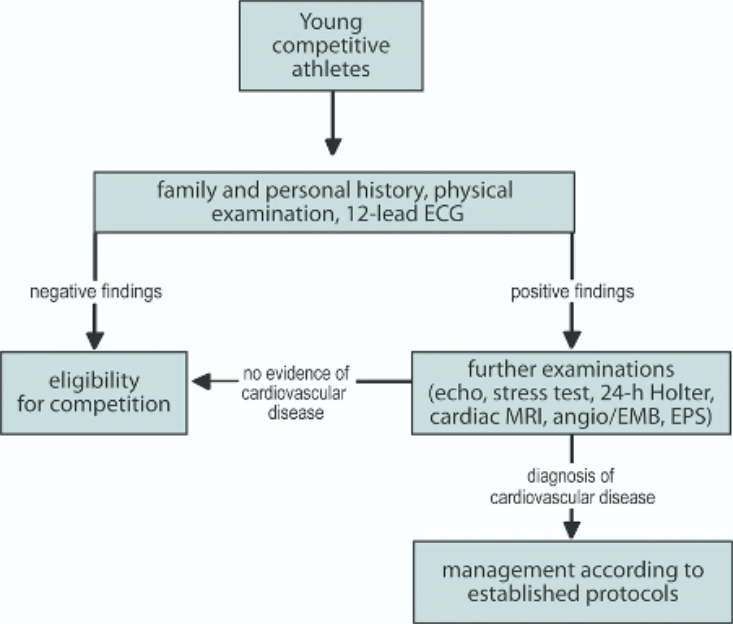
A child with chest pain must be examined, primarily to check their vital signs and conduct a cardiovascular examination, including examination of the abdomen and respiratory organs.
Sometimes it is necessary to conduct more complex medical examinations (ECG, ultrasound of the heart, stress test), as well as targeted laboratory tests (troponins, pro BNP).
Often the diagnosis is made only on the basis of anamnesis (talking to the child and parents), although in many cases the cause of chest pain cannot be determined.
In addition to the above mentioned, the task of the doctor is to assure the patient and family that the child is not in danger (after excluding serious cardiac disease) and to introduce appropriate treatment (analgesics, antacids, anti-allergy drugs...).